Your body’s silent battle with glucose could turn deadly. Learn how diabetes orchestrates a devastating chain reaction throughout your system.
The silent killer lurks in the bloodstream of millions, wreaking havoc on bodies while victims often remain unaware. This sneaky metabolic menace goes by the name of diabetes, and it’s not playing nice with anyone’s health. Whether it’s type 1, type 2, gestational, or prediabetes, the core problem remains the same – the body’s relationship with glucose has gone seriously wrong.
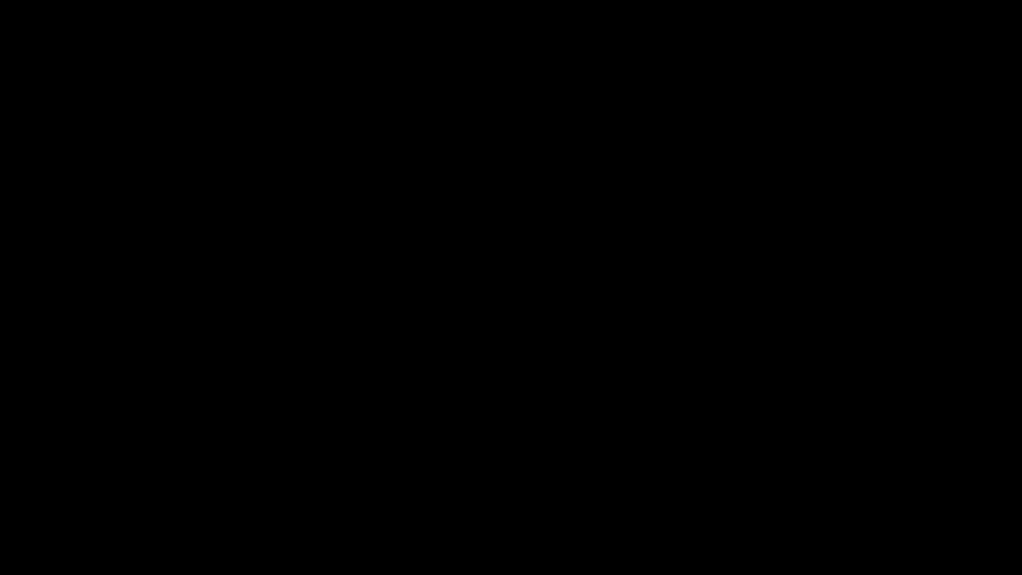
Think of insulin as your body’s bouncer, helping glucose get into cells where it belongs. But in diabetes, this bouncer either goes AWOL (type 1) or becomes incredibly ineffective at its job (type 2). The result? Glucose parties in the bloodstream instead of powering cells. And boy, does that cause problems. Making lifestyle modifications early can help prevent diabetes from developing in those at risk.
The warning signs are there, if you’re paying attention. Constant bathroom trips? Check. Thirst that won’t quit? You bet. Blurry vision and feeling like you’ve been hit by a truck? Classic diabetes red flags. Type 1 diabetes crashes the party quickly, while type 2 sneaks in like a thief in the night, sometimes taking years before anyone notices. Nearly 74% of diabetic adults also battle with high blood pressure, making their health challenges even more complex.
Diabetes announces itself with unmistakable signs – excessive thirst, frequent urination, and fatigue. Some forms strike fast, others lurk silently.
But here’s where it gets really nasty. Those elevated blood sugar levels are like sandpaper on your blood vessels, slowly but surely scraping away at their health. Heart disease? More likely. Strokes? You’re at higher risk. Your eyes? They’re taking a beating too, with diabetic retinopathy threatening to dim the lights permanently.
The damage doesn’t stop there. Nerve endings start going haywire, sending phantom tingles through extremities or, worse, no signals at all. Skin gets into the act, healing slower than a snail’s pace and practically rolling out the welcome mat for infections. If left untreated, slow-healing sores can become a serious complication requiring immediate medical attention.
And let’s not forget the kidneys – they’re working overtime, trying to filter out the excess sugar while slowly losing the battle.
The good news? Knowledge is power, and catching diabetes early can help prevent its worst effects. Regular check-ups, maintaining a healthy weight, and staying active are your best weapons against this metabolic miscreant.
Frequently Asked Questions
Can Diabetes Be Cured Completely Through Lifestyle Changes and Medication?
Diabetes can’t be completely cured, but it can be reversed – there’s a difference.
Through lifestyle changes like diet, exercise, and weight loss, some people can achieve normal blood sugar levels without medication.
Type 2 diabetes responds better to these interventions than Type 1.
Medications help, but they’re not a magic fix.
The key? Commitment to long-term changes.
No shortcuts here, folks.
Is Diabetes Genetic, and Can It Skip Generations?
Diabetes definitely has a genetic component – blame your parents for that one.
Type 2 diabetes shows strong hereditary patterns, with multiple genes playing troublemaker.
But here’s the thing: it doesn’t technically “skip” generations. Those genetic predispositions are always there, lurking.
Whether they activate? That’s where environment comes in.
Having diabetic parents cranks up lifetime risk to 40%, and if both parents have it – welcome to the 70% club.
Why Do Some Diabetics Need Insulin While Others Take Pills?
It’s all about the type of diabetes someone has.
Type 1 diabetics? Their pancreas is basically on permanent vacation – no insulin production whatsoever. They need injectable insulin to survive, period.
Type 2 diabetics still produce insulin, but their bodies are just being stubborn about using it. Pills can help wake up those lazy cells and improve insulin sensitivity.
Sometimes, Type 2s might eventually need both.
At What Age Can Type 1 Diabetes First Develop?
Type 1 diabetes can strike at any age – from infants to seniors. No one’s immune.
While it typically shows up in kids and teenagers, with peak times around ages 4-7 and 10-14, adults aren’t off the hook. Some people don’t develop it until their 30s or later.
That’s right – being an adult doesn’t protect you. The onset can be sudden or gradual, but once it hits, it’s a lifelong companion.
Can Stress and Anxiety Trigger Diabetes in Otherwise Healthy People?
Yes, stress and anxiety can trigger diabetes in susceptible individuals.
The science is clear – prolonged stress releases hormones that mess with blood sugar and insulin sensitivity. Chronic stress leads to insulin resistance, a major precursor to type 2 diabetes.
Throw in stress-related poor eating habits and reduced exercise, and you’ve got a perfect storm. Not everyone under stress develops diabetes, but it’s definitely a risk factor.









8 comments