While specialists might get all the glory, it’s America’s primary care doctors who are drowning in diabetes cases. These frontline physicians handle more than 90% of diabetes management nationwide. That’s not a typo—ninety percent. The burden is crushing, and it’s only getting worse as 38.4 million Americans now live with the disease.
Primary care wasn’t built for this. The math doesn’t add up: too many patients, not enough time. A doctor might have fifteen minutes to address multiple medications, lifestyle changes, comorbidities like hypertension, and whatever other complaints the patient walked in with. Good luck with that.
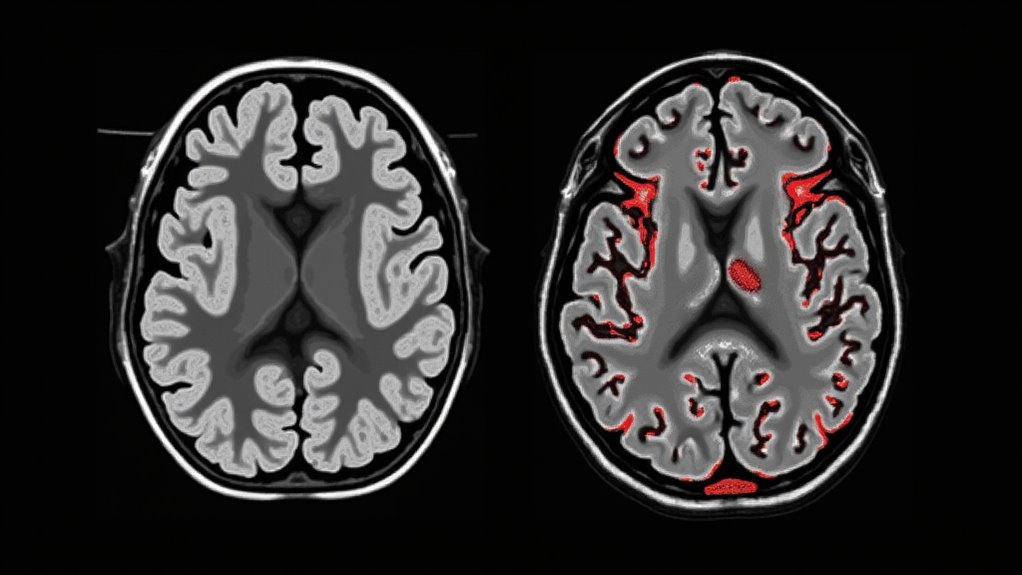
The diabetes crisis crammed into a 15-minute appointment—an impossible math problem with human consequences.
The shortage of endocrinologists isn’t helping. Patients who should see specialists can’t get appointments, so guess who picks up the slack? Your overworked family doctor, that’s who. Understanding type 1 versus type 2 diabetes requires different treatment approaches, making the physician’s job even more complex.
Many physicians admit they lack confidence in starting insulin therapy or coaching lifestyle changes. Can you blame them? Their training often skimps on these skills. But diabetes doesn’t care about your medical school curriculum.
The financial side is equally bleak. The payment system wasn’t designed for complex chronic disease management. Doctors need teams—nurses, dietitians, health coaches—but who’s paying for that? Not the current reimbursement model.
Studies show team-based care works. Patient-centered medical homes and chronic care models improve outcomes. But implementing these approaches requires resources many practices simply don’t have.
Meanwhile, the diabetes tsunami grows. An aging population. Rising obesity rates. The perfect storm.
Social factors complicate everything. Poverty. Food deserts. Language barriers. These aren’t medical problems with medical solutions, yet they land on the primary care doorstep. The disparities in care access disproportionately impact racial and ethnic minorities, creating another layer of challenges for already strained primary care providers.
Some clinics are finding ways to adapt. Technology helps. So does better training. Interdisciplinary teams make a difference when practices can afford them.
But the system needs an overhaul. Primary care can’t continue bearing this weight without fundamental changes. The doctors are tired. Their patients deserve better. Something’s gotta give.